Why are we still talking about volatile anaesthesia? Why do anaesthetists feel comfortable with sticking to old practice and don’t feel the need to progress? And why does the medical literature offer so little to support this change?
I remember when I was teaching a trainee during the end of last year. He was fairly advanced in his training and knew about pharmacology the best of what is required for the exam and beyond. We were in cardiac theatre and I was asking him about his consideration regarding the choice of anaesthetic drugs. He knew I was expecting a favourable portrait of TIVA but I asked him to challenge me with anything good he can think of about volatiles.
We then talked about almost everything from cardio-protection, organ toxicity, PONV, recovery times to physiologic regulation and effects on the endothelium and the inflammatory response. We discussed the most cited studies and debated the details in each paper until we ended in an exhausted stalemate whether or not translational research will ever have a tangible meaning for the individual patient and indeed the anaesthetist in theatre.

We came to the following two conclusions on volatile agents and their presumed benefit:
- There are very few proof-of concept studies on patients.
- None of the high-profile claims are consistently seen in patient cohorts.
In this sense, it became clear that research in anaesthetic pharmacology quite often is a rather detached matter from patient care and of daily practice from which clinicians can draw advice from.
The bulk of literature comparing TIVA with volatiles is based on mechanistic deduction for a perceived purpose. Why on earth does anybody think a slightly less enhanced IL6 response to lung surgery in 25 patients does say anything we can conclude on. Do the perioperative troponin levels and their small differences really mean a patient will be worse off? Is it the patient's individual response rather than the intervention that influences the results? The mechanism and dynamics of anaesthesia is still so poorly understood in its own right that it is hard to conceive that derived mechanisms have any meaning let alone impact on hard outcomes like mortality.
Are we asking the right questions?
The missing piece in this research conundrum in my view is the patient itself. Very little effort is made to ask what is best for the patient, what will improve the patients condition and progress. What do patients think has improved or jeopardised their recovery from surgery? What actually happens to our patients?
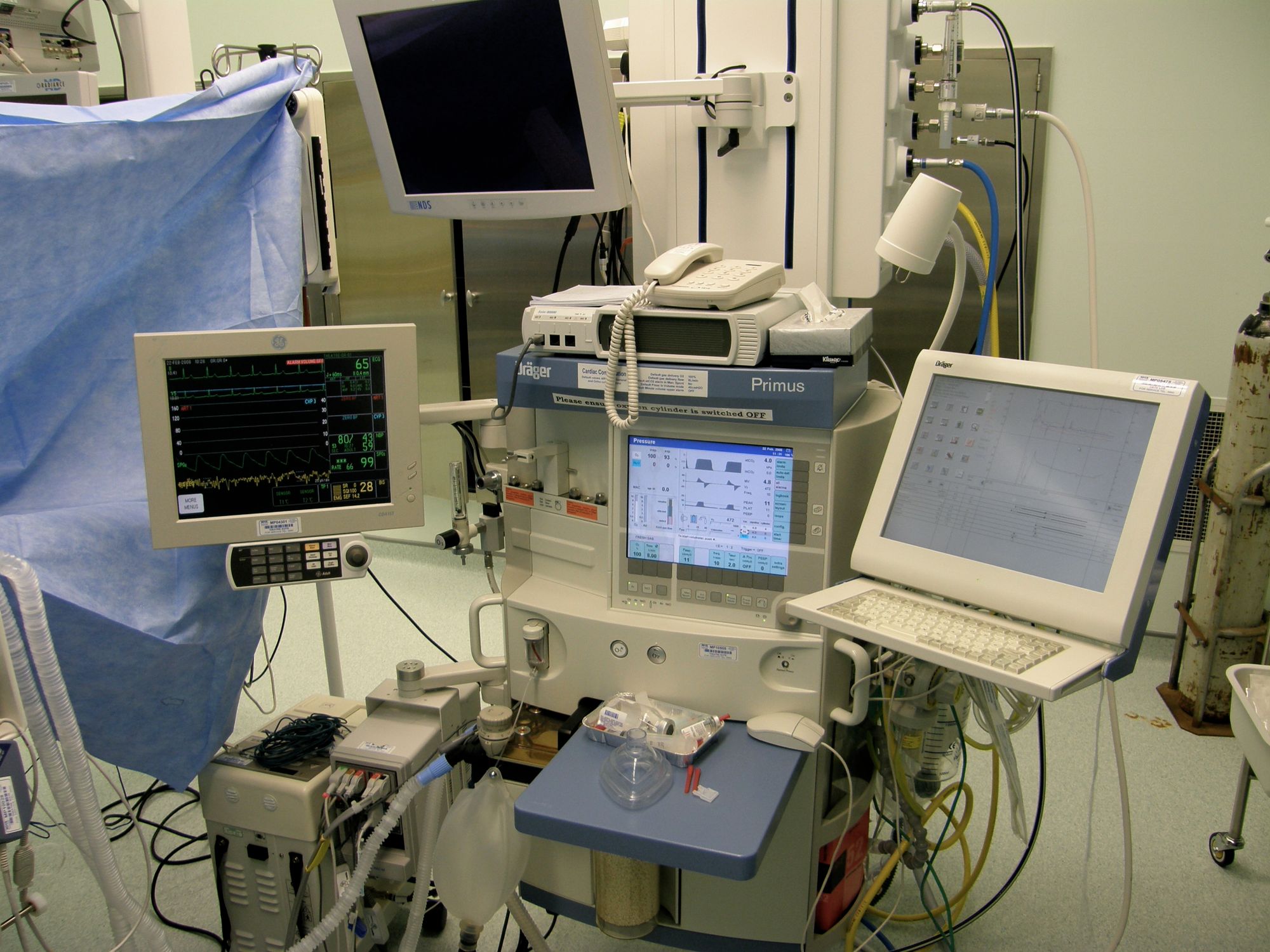
So is it time to dial down the vaporiser as Marcel Durieux suggested in his editorial from 2015 in the British Journal of Anaesthesia (BJA 2015;114:715-6)? Or, taking it a bit further, is there any good reason of still having them attached to the anaesthetic machine?
In this editorial he comments on the possible effect some components of our anaesthetic, in particular volatile agents, may have on the promotion of cancer cells and hence the ultimate impact on survival of the patients that we anaesthetise. Similar concerns were discussed when data became available linking the exposure to volatile agents with a higher likelihood of developing neurodegenerative disease, such as Alzheimer’s.
Since then, a lot more topics have been screened on the merit or concern with volatiles, like actual cancer outcomes and postoperative delirium. Yet, patient studies still deliver ambiguity and retrospective research from registries, however convincing they might look, are failing us in real world evidence.
Simple extrapolation of experimental and animal data is difficult and the medical community is still devoted to the power and ultimate verdict that comes from prospective RCTs in typical patient cohorts. But even then, we are never sure.
As far as we currently know, modern intravenous anaesthesia, which is pretty much synonymous to continuous propofol and remifentanil infusion via TCI has eliminated many unpleasant and sometimes hazardous effects of volatile anaesthetics. Combined with the use of appropriate local anaesthetic techniques, TIVA has enhanced the well-being of our patients, facilitates improvements in theatre management and has so far not shown any serious long-term effects on overall survival. Institutions that have adapted TIVA as their choice for surgical anaesthesia and sedation, have witnessed a transformation in peri-operative care. And the discussion of the environmental impact of volatiles is gaining track. Why bother with volatiles any more?

So, ultimately, it’s time to do the final step and remove the vaporisers. Our patients will love it.
The following day my trainee did a thoracotomy using TIVA and a high thoracic epidural and had a good day with one of his most satisfied patients.
