The incentive of these pharmacokinetic DiY blogs was to give colleagues that have an interest in pharmacokinetics and pharmacodynamics a relative simple tool to use published pk/pd models and make simulations that can be used to deepen the understanding of the tools like TCI that we use in daily practice to perform anaesthesia. We have used the Euler approximation in a spreadsheet and demonstrated that small steps of 5 seconds could be sufficiently closely matched to the exponential equations and graphs that represent the evolution of drug concentrations in a patient. This was possible for bolus, infusion and target controlled infusion in a deterministic way, in other words: based on calculations that are simple and valid for all drugs simulations.
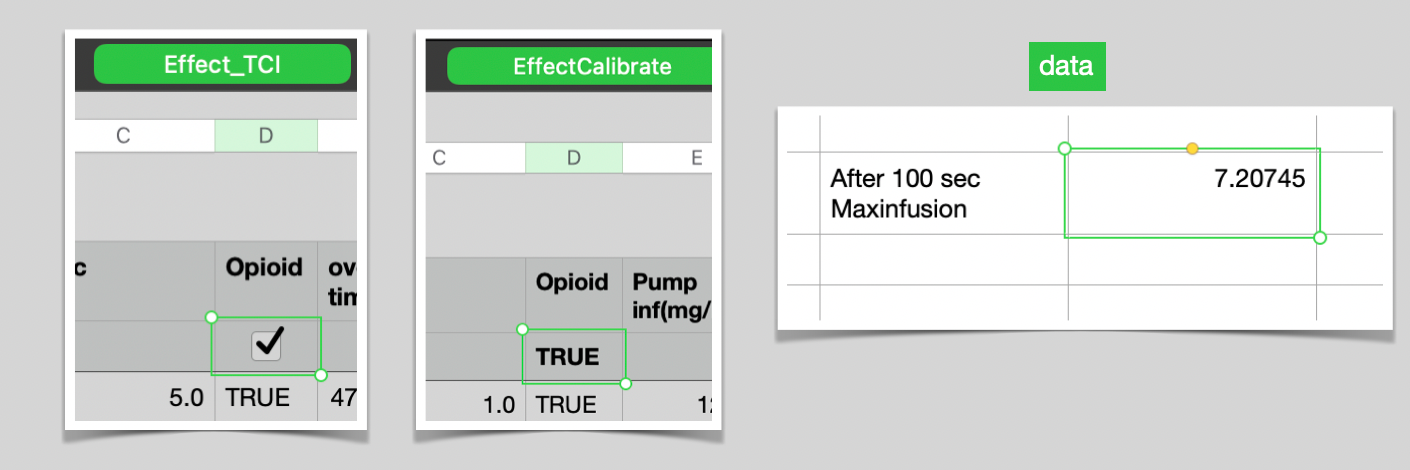
For me these spreadsheets are valuable despite the fact that I have developed Tivatrainer(X) that uses analytical equations and is in theory more accurate. For a quick simulation to verify an idea or concept I still use the spreadsheet approach because it will allow the use of any model not just compartimental. The principle of a spreadsheet is that in every row a small linear step of a complex process is performed while the input comes from another previously calculate row or cell. This is not sufficient for effect compartment control as this requires a forward looking algorithme: run the pump on maximum speed untill after stopping the blood and effect site concentration equilibrate to the required target without over or undershoot of the effect compartment concentration. Steve Shafer proposed a calibration dose in his book on IV anesthesia: give a bolus, look at the peak effect: this is where blood and effect equilibrate and note the overshoot of the blood concentration. Because pharmacokinetics are assumed to be linear(2 x dose -> 2 x concentration) you can work out the required bolus for a given effect. TCI systems use infusions not bolusses so this approach will not work. But the calibration concept is usable for the proposed heuristic solution. In the spreadsheet there is an 'EffectCalibrate' sheet. Infusion is given at a maximum rate specified in the 'data' sheet. After 100 seconds the infusion is stopped and the maximum effect site concentration(this is the equilibrium between effect and blood) is stored also in the 'data' sheet. These calculations in the 'EffectCalibrate' sheet can be done with or without opioid pk. An interval of 1 second is used in the 'EffectCalibrate' sheet to minimise the inaccuracy that is caused by the the Euler technique of stepwise change. For Propofol this 1 second is acceptable but for other drugs running the infusion at maximum speed for 1 second too short or too long will create a too big deviation and the stepsize possibly should be decreased. Then the peakeffect is used to calculate the time the maximum infusion has to run to achieve the required calculation using the calculation:
\(Time_{MaxInfuse}= (Target / PeakEffect * 100 -1\)) sec
With some if statements this calculation is activated only when there is an increase in target. For the remaining, effect TCI and blood TCI is similar appart from a decrease in the target, then the infusion is stopped until the effect concentration equals the target. This works suprisingly well when super imposed on the existing TCI calculations.
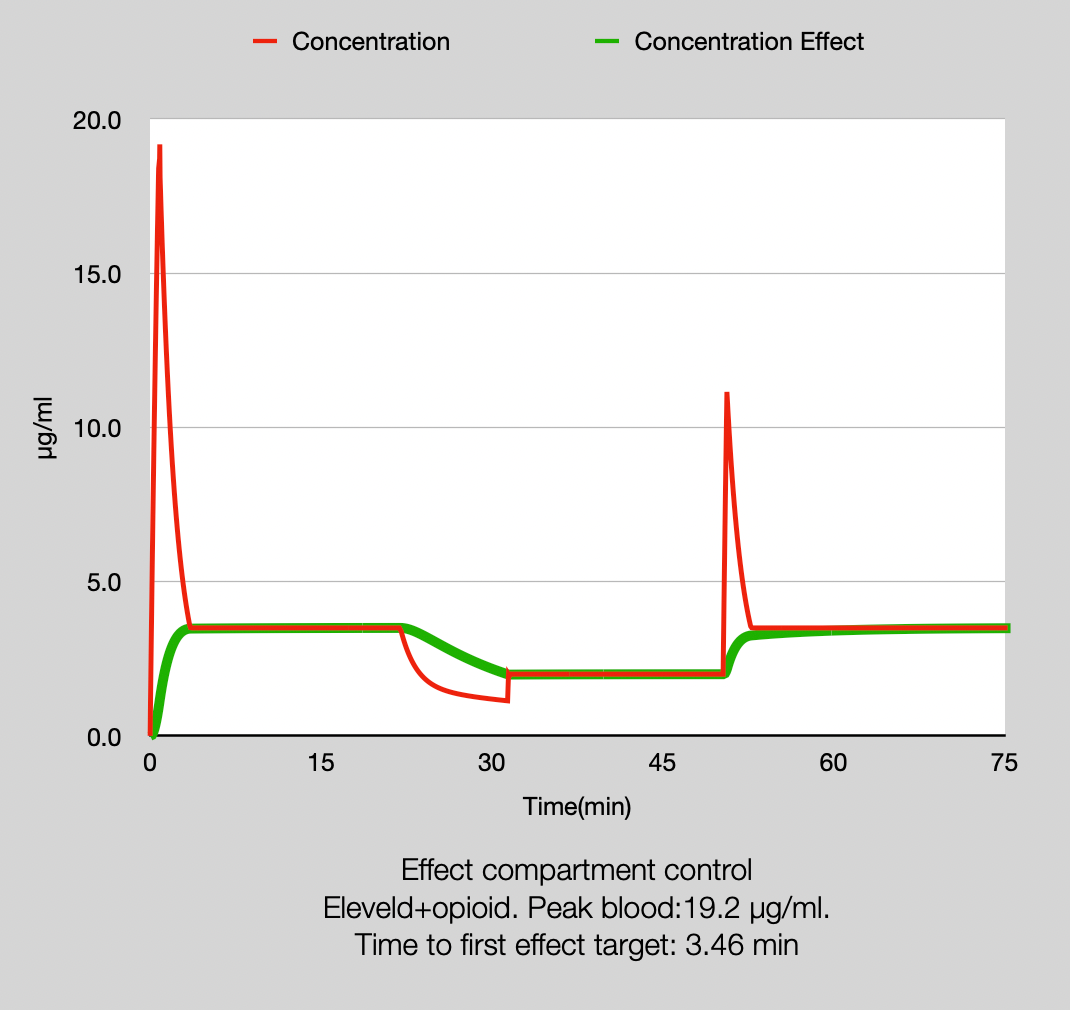
You may notice a small undershoot in the second target increase. This is because opposite to the linear Pk for boluses this is not valid for infusions. Nevertheless this heuristic model serves our purpose well. When compared with a TivatrainerX simulation the total amopunt given by the spreadsheet after 91.6 minutes was 858 mg versus 856 mg predicted by Tivatrainer.
Now the induction scenario, presented in the previous DiY blogs can be worked out for effect compartment control: the TCI device uses the Eleveld model with opioid but the patient receives the opioid only after 5, 10 or 15 minutes. So for that period the pharmacokinetics of the propofol in the patient do not match the used pharmacokinetics in the TCI system. In blog DiY3 this is worked out for (effect compartment) concentration and BIS using blood control TCI, in this spreadsheet it is worked out for effect target controlled infusion.
How it works:
-after setting the target in Effect_TCI check the opioid tickbox in effect_TCI.(set it to 'true' in excel) This will automatically also set the opioid pk in EffecCalibrate sheet to true and in the data sheet the maximum effect site concentration after 100 minutes running maximum infusion rate is stored(7.20745 µg/ml)
Based on the above equation the duration of the infusion running on max for the target is calculated.
The infusion rates produced by this simulation[column G] are now copied and the formula results (or values excel) are pasted into the induction sheet[column F]. See blog DiY3 for a more detailed instruction. All the spreadsheets use 5 second intervals. For the effect compartment control an adaptation is built in to adjust the last step otherwise the maximum infusion rate could run 5 seconds too long or too short.
Therefore you will have to copy the step in the sec column (column C) to the sec [column C] in the induction sheet. Again paste the formula results (values in excel]
If you check all the rows in the opioid[column D](= use opioid Pk) the the effect compartment concentration should nicely match the target. For our scenario uncheck the rows in the opioid[column D] for the respective period of time : 5, 10 or 15 minutes and for each step copy the concentration, effect site concetration and Bis to a column for graphing. Again paste formula results (values in excel)
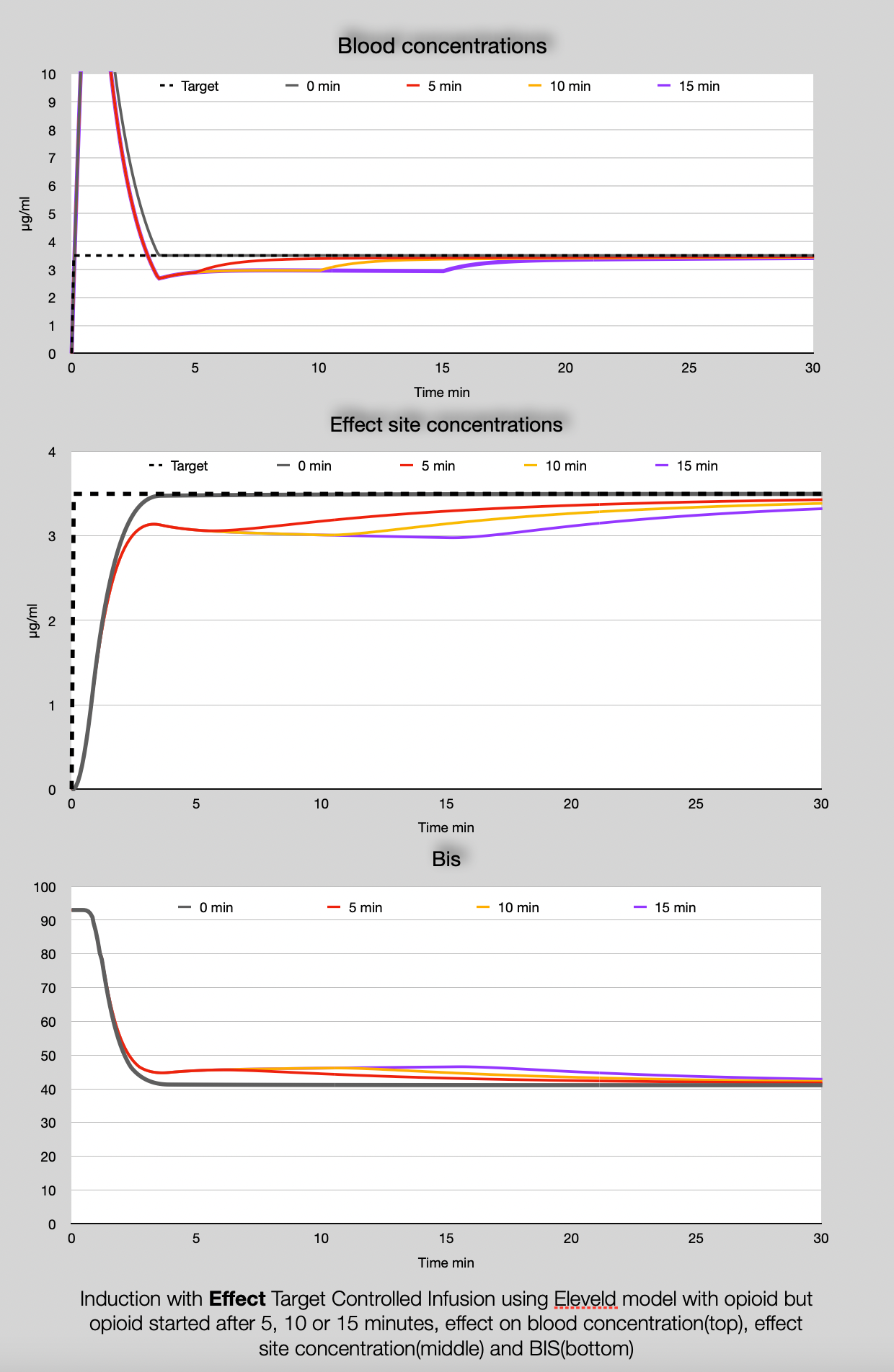
There is a considerable undershoot in the blood concentration AND effect site concentration due to the fact that mainly the clearance of propofol is higher than the ETCI systems calculates. However in the effect : the BIS, this is smoothed out. It has been said in the previous blog: these are simulations based on extrapolated data. In reality the effects maybe or maybe not noticable, but if you notice differences these simulations may help to understand the origin of the differences. If you select a little bit higher target for induction and a bit lower once the opioid has been started you may (in theory) adjust for the effect for the later start of the opioid but as more factors determin how adequate your anesthesia is (Pd interaction with other drugs, surgical stimulus, hemodynamic changes) adjusting the target based on these simulation is possibly a control overshoot.
The biggest advantage of the Eleveld model is that clinicians do not have to worry about the validity of the model for different patients. You can use it for old, young, and obese patients with no need to 'patch' the input. Using TCI then resembles more the inhalational technique. The question is if the availability and implementation of two different models, with and without opioid really contributes to the ease of applying intravenous anesthesia and if it would not be better to leave the (model) adaptation to the titration skills of the anaesthesiologist. Cardiac output changes the uptake of inhalational agents. Opioids (and other drugs and intraoperative events) change the cardiac output so for that only, adjustments of the vaporiser settings are required and anaesthesiologist are familiar with doing so: it is part of their professional skills. Are we not witnessing another example of theoretic reasoning being forced into practice without observed or demonstrated clinical benefits while facing again the confusion that it wil generate? It is up to you to answer this.
Happy thinking!
Again like has been said in previous blogs: If you use this material than please disclose the source as an appreciation of my work:
Frank Engbers at Eurosiva
Please use the box below for comments and questions. Messages can be sent anonymously.
Downloads:

